
10 Despite these efforts, a consensus for this relationship has not been achieved because of conflicting evidence. 5- 10 Some studies have analyzed electronic health records in Britain, 5 Denmark, 6 Canada, 7 and Sweden 8 through retrospective cohort or case-control designs, whereas others have analyzed adverse event reports through drug surveillance 9 or disproportionality methods. The relationship between antidepressants and hyponatremia has been studied extensively in recent years. Therefore, it is clinically important to identify antidepressants that are less likely to cause hyponatremia. 3, 4 As these symptoms overlap with those of depression, antidepressant-induced hyponatremia may go unnoticed and could lead to life-threatening consequences.
1, 2 Hyponatremia is one such adverse effect, with symptoms ranging from mild lethargy and anorexia to severe seizures and coma. However, recent studies have shown that some adverse effects are more pronounced in new-generation antidepressants. Among the different antidepressants, new-generation antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-noradrenaline reuptake inhibitors (SNRIs), are recommended as first-line treatment because they are believed to be safer than the older tricyclic antidepressants (TCAs). ☑ Our study provides clinically useful information for optimizing current antidepressant therapy as well as pharmacologically important insights for developing safer antidepressants in the future.Īntidepressants are commonly used to treat depression and other disorders in clinical practice. HOW MIGHT THIS CHANGE CLINICAL PHARMACOLOGY OR TRANSLATIONAL SCIENCE?.☑ Mirtazapine, fluvoxamine, and milnacipran are less likely to cause hyponatremia because of (i) no lowering effect on serum sodium levels, (ii) no significant increase in hyponatremia reports, and (iii) lower binding affinity for serotonin transporter capable of explaining (i) and (ii). WHAT DOES THIS STUDY ADD TO OUR KNOWLEDGE?.☑ This study aimed to identify antidepressants that are less likely to cause hyponatremia through triangulation of retrospective cohort, disproportionality, and pharmacodynamic studies. However, owing to conflicting evidence regarding specific antidepressants, it is unclear which antidepressants are less likely to cause hyponatremia. ☑ Antidepressant-induced hyponatremia is a potentially life-threatening adverse effect. WHAT IS THE CURRENT KNOWLEDGE ON THE TOPIC?.Although further research is needed, our data suggest that mirtazapine, fluvoxamine, and milnacipran are less likely to cause hyponatremia. Finally, pharmacoepidemiological–pharmacodynamic analysis revealed a significant correlation between the decrease in serum sodium levels and binding affinity for serotonin transporter (SERT r = −0.84, P = 0.02), suggesting that lower binding affinity of mirtazapine, fluvoxamine, and milnacipran against SERT is responsible for the above difference. In the disproportionality analysis of patients (≥ 60 years) in the Japanese Adverse Drug Event Report database (2004–2020), a significant increase in hyponatremia reports was observed for SSRIs (reporting odds ratio 4.41, 95% confidence interval 3.58–5.45) and SNRIs (5.66, 4.38–7.31), but not for mirtazapine (1.08, 0.74–1.58), fluvoxamine (1.48, 0.94–2.32), and milnacipran (0.85, 0.45–1.62).

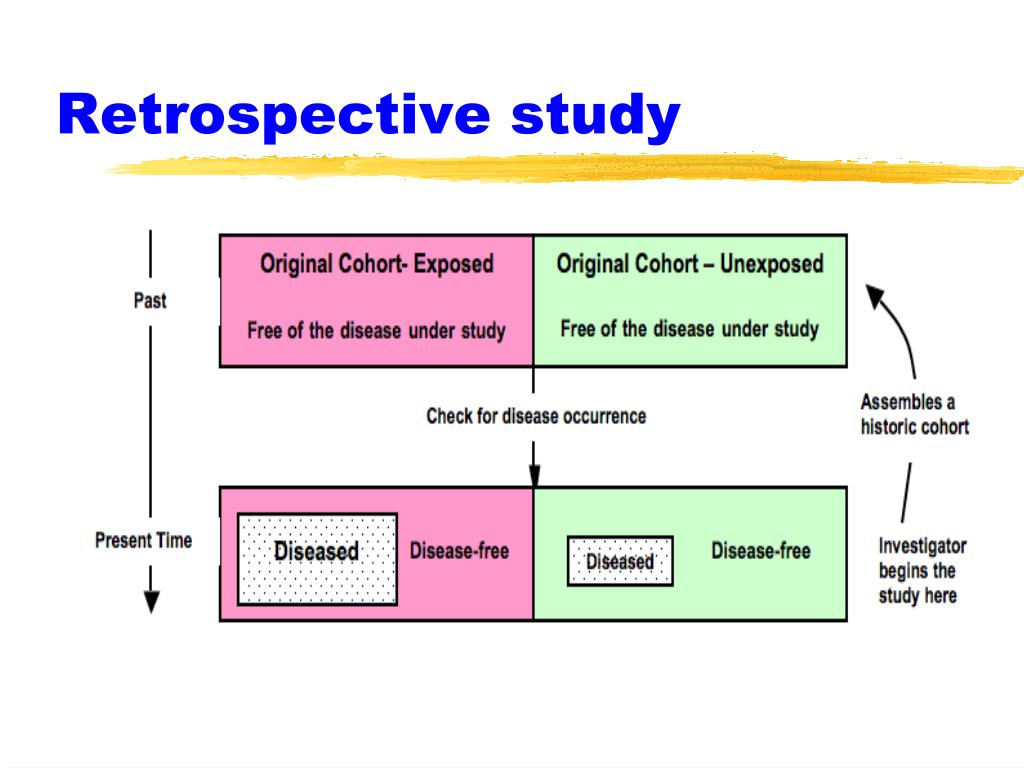
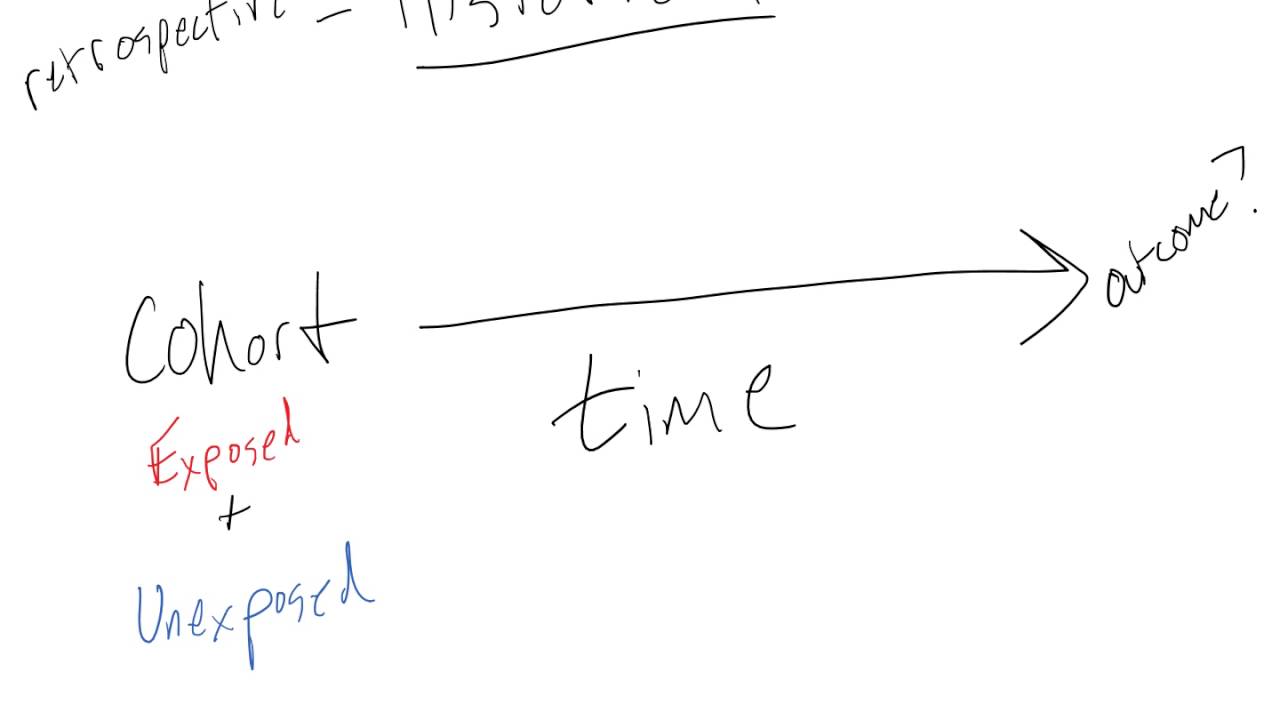
Within-class comparison revealed no decrease in serum sodium levels for fluvoxamine (+0.74 ± 0.75 mmol/L, P = 0.33) among SSRIs and milnacipran (+0.08 ± 0.87 mmol/L, P = 0.93) among SNRIs. In the retrospective cohort study of patients (≥ 60 years) in Nihon University School of Medicine’s Clinical Data Warehouse (2004–2020), a significant decrease in serum sodium levels was observed within 30 days after initiation of a selective serotonin reuptake inhibitor (SSRI mean change −1.00 ± 0.23 mmol/L, P < 0.001) or serotonin-noradrenaline reuptake inhibitor (SNRI −1.01 ± 0.31 mmol/L, P = 0.0013), whereas no decrease was found for a noradrenergic and specific serotonergic antidepressant (mirtazapine +0.55 ± 0.47 mmol/L, P = 0.24). To identify antidepressants less likely to cause hyponatremia, we conducted a triangulation study integrating retrospective cohort, disproportionality, and pharmacodynamic studies. Antidepressants are known to cause hyponatremia, but conflicting evidence exists regarding specific antidepressants.


 0 kommentar(er)
0 kommentar(er)
